Canine Atopic Dermatitis-Making itchy conversations easier.
Canine atopic dermatitis (cAD) is everywhere being one of the most common causes of pruritic dermatitis in the dog. Some epidemiological data suggests that upwards of 15% of the dog population is affected by environmental skin allergies. Recent advances in our understanding of the disease have ushered in an exciting new era of non-steroidal antipruritic medications that can effectively and safely manage allergy signs in some dogs. We now appreciate, however, that canine atopic dermatitis is a clinical syndrome (rather than a single disease entity) affecting each dog in a unique way. As such a ‘template’ approach often leads to treatment failure; our patients deserve an individualised treatment regimen tailored to their specific needs.
What exactly is canine atopic dermatitis?
This condition is defined as, “a genetically predisposed inflammatory and pruritic dermatitis with characteristic clinical features associated with allergen-specific antibodies (IgE) directed against environmental triggers.” Quite the mouth full! Essentially, canine atopic dermatitis is an allergy to environmental triggers (pollens, moulds, danders, house dust mites) arising from the complex interplay of genetic and environmental factors that shape the cutaneous immune response and skin barrier function (or dysfunction, as the case may be).
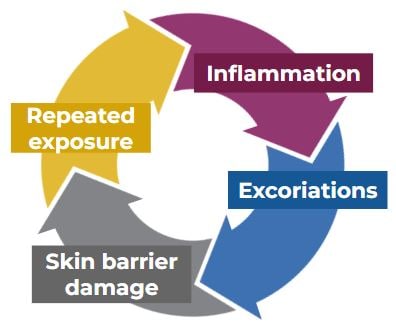
Abnormal genes and environmental stressors perpetuate immune dysfunction (loss of tolerance) and skin barrier dysfunction which, in turn, allows for microbial dysbiosis, allergen penetration and neuronal sensitisation. The result is the characteristic and frustrating vicious cycle of itch, recurrent infections and impaired quality of life. Optimising outcomes on the clinic floor necessitates that we attend to both the immune and skin barrier dysfunctions in our patients.
Diagnosing canine atopic dermatitis
There is no one diagnostic test we can rely upon to make a diagnosis of canine atopic dermatitis. Our index of suspicion for allergic dermatitis (food and/or environmental allergy) is increased when an often-exasperated client tells us of their dog’s itch (manifesting as excessive licking, biting, chewing, pawing, gnawing, shaking, scratching, rubbing, scooting behaviours) with a characteristic distribution on exam (paws, muzzle, ears, groin, armpits, amongst others). Then we rule out conditions that can mimic canine atopic dermatitis including ectoparasitism (skin scrapes) and dermatophytosis (Wood’s lamp exam, hair plucks, fungal culture +/- PCR tests). Always assess for secondary infections (in-house cytologies) that can be complicating the clinical picture. We rule out a cutaneous food allergy (presuming allergy signs are non-seasonal) with a strict elimination diet trial. Finally, we confirm a diagnosis of cAD when the patient fails to respond to the diet trial or in the absence of a flare on provocative diet re-challenge.
With a diagnosis we can formulate a treatment plan adhering to the following tenants:
- Identify and avoid allergy triggers (easier said than done; aeroallergens cannot be realistically avoided by our patients);
- Improve the skin barrier; and
- Reduce pruritus and skin lesions.
Treatment for cAD
The gold standard treatment for cAD remains allergy testing and immunotherapy (desensitisation). Always consider sending atopic patients to your local veterinary dermatologist for this discussion. In the absence of immunotherapy, or while awaiting response to this intervention, each patient requires symptomatic therapy to ameliorate the itch. Manage immune dysfunction with an anchor antipruritic feasible for the client and tolerable for the patient (e.g. Apoquel, Cytopoint, steroids, Atopica). Concurrently, attend to barrier dysfunction with omega 6 fatty acids. I recommend feeding Hill’s Derm Complete which both minimises allergic dermatitis and bolsters the skin barrier with its mix of EFAs, phytonutrients and bioactives. Remember to keep secondary infections at bay with weekly topical antiseptics (e.g. dilute chlorhexidine shampoos and conditioners). Finally, allergic otitis and pododermatitis often prove refractory to systemic non-steroidal antipruritic therapy, so incorporate a topical steroid (e.g. Cortavance) twice weekly for the ears and paws to prevent localised allergy breakthrough.